Medical researchers have discovered that laying the smackdown on DNA’s cousin – RNA – might help put a stop to the development of degenerative eye disorders.
And by smackdown, we mean that UT Southwestern Medical Center researchers have found that blocking two tiny molecules of RNA seems to put a halt to the irregular growth of blood vessels that happens with degenerative eye disorders.
Their findings are available in the Proceedings of the National Academy of Sciences, and they put forward a potential method to treat age-related macular degeneration (AMD). AMD is a vascular eye disorder that afflicts nearly 2 million Americans and it is a leading cause of blindness among older people.
“MicroRNAs can affect multiple pathways involved in age-related macular degeneration,” explained Dr. Shusheng Wang, assistant professor of ophthalmology and pharmacology and co-senior author of the study. “Therapeutic manipulation of microRNAs 23 and 27 may give us a way to treat choroidal neovascularization in patients with degenerative retinal diseases.”
Researchers found in their study that muzzling the microRNA cluster members miR-23 and miR-27 slowed down the unwarranted formation of blood vessels in the back of the eyeball, known as choroidal neovascularization.
Once these blood vessels hemorrhage and leak, it leads to a sudden weakening of central vision.
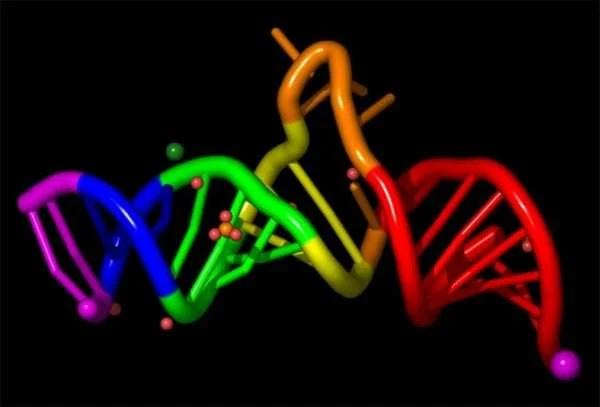
MicroRNAs are minuscule pieces of genetic material that can pinpoint multiple components of signaling pathways. By networking with other protein-making molecules in cells, they help fine-tune the expression of networks of genes and regulate cell function.
However microRNAs also can add to the excessive blood vessel formation that is the cause for vascular disorders, the current UT Southwestern study shows. That’s because they stimulate the growth of new blood vessels from pre-existing vessels, a process called angiogenesis, which is an important natural process in the body used for healing and reproduction.
The human body usually regulates angiogenesis through an exact balance of growth and inhibitory factors in healthy tissues, said Wang. When the process comes to be unbalanced, however, amplified angiogenesis can lead to a variety of incapacitating conditions.
Earlier ways of treating degenerative eye disorders have focused on limiting vascular endothelial growth factor (VEGF), a secreted protein that encourages blood vessel formation. VEGF has been known to be a causative factor in vascular disease in the retina of the eye.
Anti-VEGF drugs, which are shockingly injected into the eyeball, have been used to give patients some upgrading in vision. These drugs, nevertheless, have limited efficiency in treating some forms of neovascular AMD, and also have potential side effects.
Wang noted additional research could show that other microRNAs might also be involved, and that pursuing multiple pathways may provide benefits in the treatment of these diseases.
“We want to see if a combination of microRNAs and angiogenetic drugs have a synergetic effect on the progression of macular degeneration.”
For those interested in degenerative eye disorders, this might be one to look into.